New Enrollment Website Starting January 2026
Have a wonderful holiday and feel free to reach out to us after the first of the year with any questions or assistance.
New Cash Back/Copay Map
PEHP is doing their part to assist us to keep our claim costs down. This will help the District maintain the best medical plan possible and limit premium increases. If you participate in this program it saves both you and our plan money. PEHP has made updates to a program so you can either get cash back or pay a minimal $45 copay for high cost services. If you have met your out-of-pocket maximum the cash back is still available.
PEHP recently launched the Cash Back/Copay map to help members quickly identify where to go for the best value. It’s based on common surgeries and imaging procedures that can be done outside of a hospital facility, such as knee surgeries, colonoscopies, MRIs, and more. This new program runs alongside existing benefits to reward employees for making smart choices with their healthcare.
Here’s how it works when a member gets service at a facility included in this program:
(Automatic — No application needed)
- Pay no more than $45 copay for all services — no deductible, no hidden fees.
- Always earn cash back for certain preventive services (e.g., colonoscopy) at select locations.
- After reaching Out-of-Pocket Maximum, additional cash back may be earned.
High Deductible Plan
(Application required)
- Starts with cash back, once deductible is met, pay no more than a $45 copay until out-of-pocket max is met.
- After reaching Out-of-Pocket Maximum, additional cash back may be earned.
- Always earn cash back for certain preventive services (e.g., colonoscopy) at select locations.
To access the Cash Back/Copay Map, log in to your PEHP account and look for it under the Find Providers & Costs menu.
If you have any questions, please reach out to PEHP directly 801-366-7555 or Insurance Services at 801-567-8146 or insurance@jordandistrict.org.
PEHP ID Cards
 The open enrollment and migration to PEHP's new system should now be complete. There have been many challenges and thank you so much for your patience. Many employees received multiple PEHP Member ID Cards. The Member ID Number should be the same on all cards. If you received a set of cards that does not match the plan you enrolled in, please log into PEHP and verify the correct plan is showing in their system.
The open enrollment and migration to PEHP's new system should now be complete. There have been many challenges and thank you so much for your patience. Many employees received multiple PEHP Member ID Cards. The Member ID Number should be the same on all cards. If you received a set of cards that does not match the plan you enrolled in, please log into PEHP and verify the correct plan is showing in their system.
If for some reason you see it is not correct, please contact Insurance Services / 801-567-8146 / insurance@jordandistrict.org.
PEHP – Explanation of Benefits
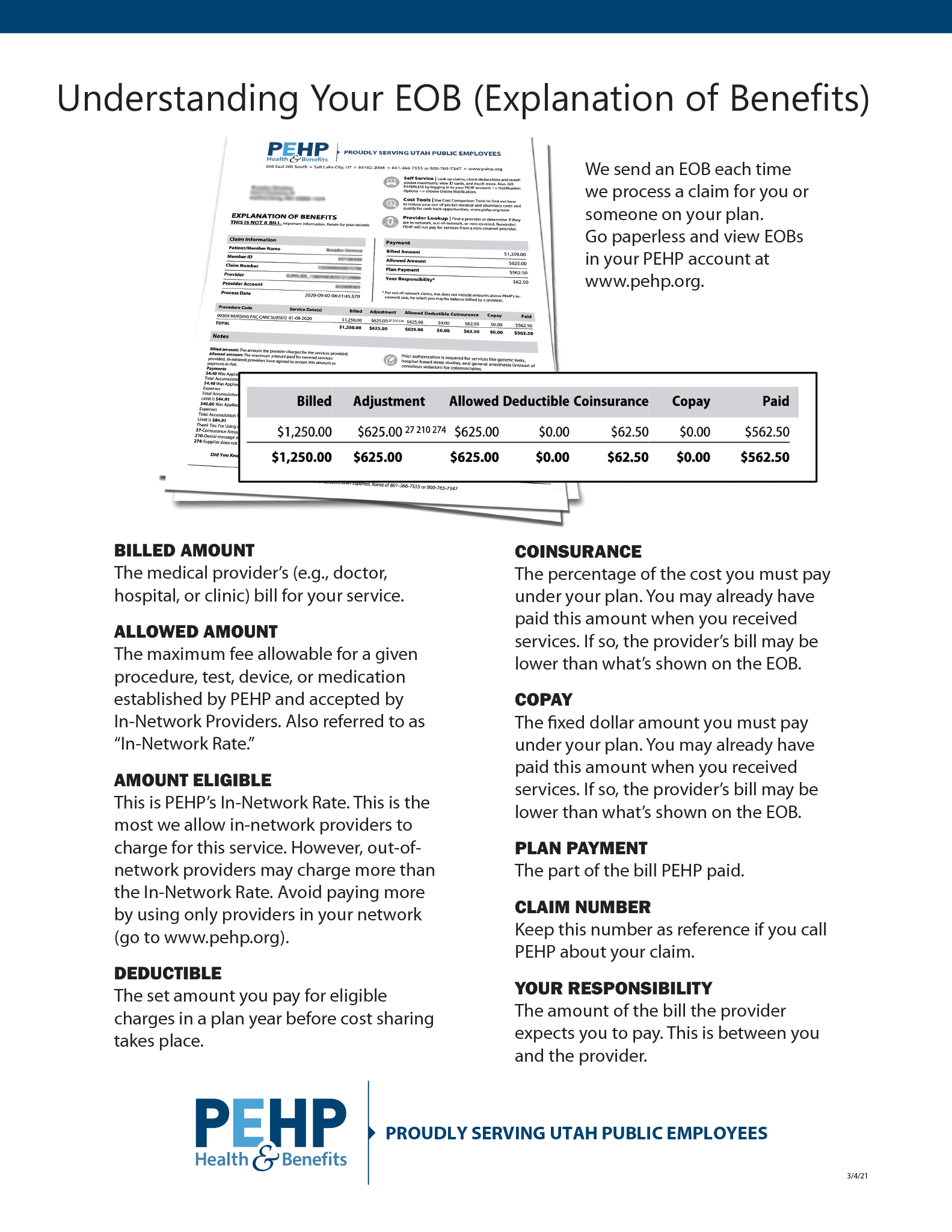 When you are using the health plan, the Explanation of Benefits (EOB) is the most important document when it comes to the billing side of your care. You either receive the EOB in the mail or you have access to them through the PEHP online portal. You elect how you receive this document.
When you are using the health plan, the Explanation of Benefits (EOB) is the most important document when it comes to the billing side of your care. You either receive the EOB in the mail or you have access to them through the PEHP online portal. You elect how you receive this document.
Once you receive this document, match it up with a bill you receive from your provider and pay what PEHP states is "Your Responsibility". It may not match what your provider's bill is showing but your provider receives the same information from PEHP. If there is a portion that is not being covered it could be that PEHP needs additional information or your provider needs to write off the balance.
- Billed Amount - The medical provider’s (e.g., doctor, hospital, or clinic) bill for your service.
- Allowed Amount - The maximum fee allowable for a given procedure, test, device, or medication established by PEHP and accepted by In-Network Providers. Also referred to as “In-Network Rate.”
- Amount Eligible - This is PEHP’s In-Network Rate. This is the most we allow in-network providers to charge for this service. However, out-of network providers may charge more than the In-Network Rate. Avoid paying more by using only providers in your network (go to www.pehp.org).
- Deductable - The set amount you pay for eligible charges in a plan year before cost sharing takes place.
- Coinsurance - The percentage of the cost you must pay under your plan. You may already have paid this amount when you received services. If so, the provider’s bill may be lower than what’s shown on the EOB.
- Copay - The fixed dollar amount you must pay under your plan. You may already have paid this amount when you received services. If so, the provider’s bill may be lower than what’s shown on the EOB.
- Plan Payment - The part of the bill PEHP paid.
- Claim Number - Keep this number as reference if you call PEHP about your claim.
- Your Responsibility - The amount of the bill the provider expects you to pay. This is between you and the provider.
Please contact Insurance Services with any questions or concerns 801-567-8146 / insurance@jordandistrict.org
Express Scripts / Evernorth Health Services
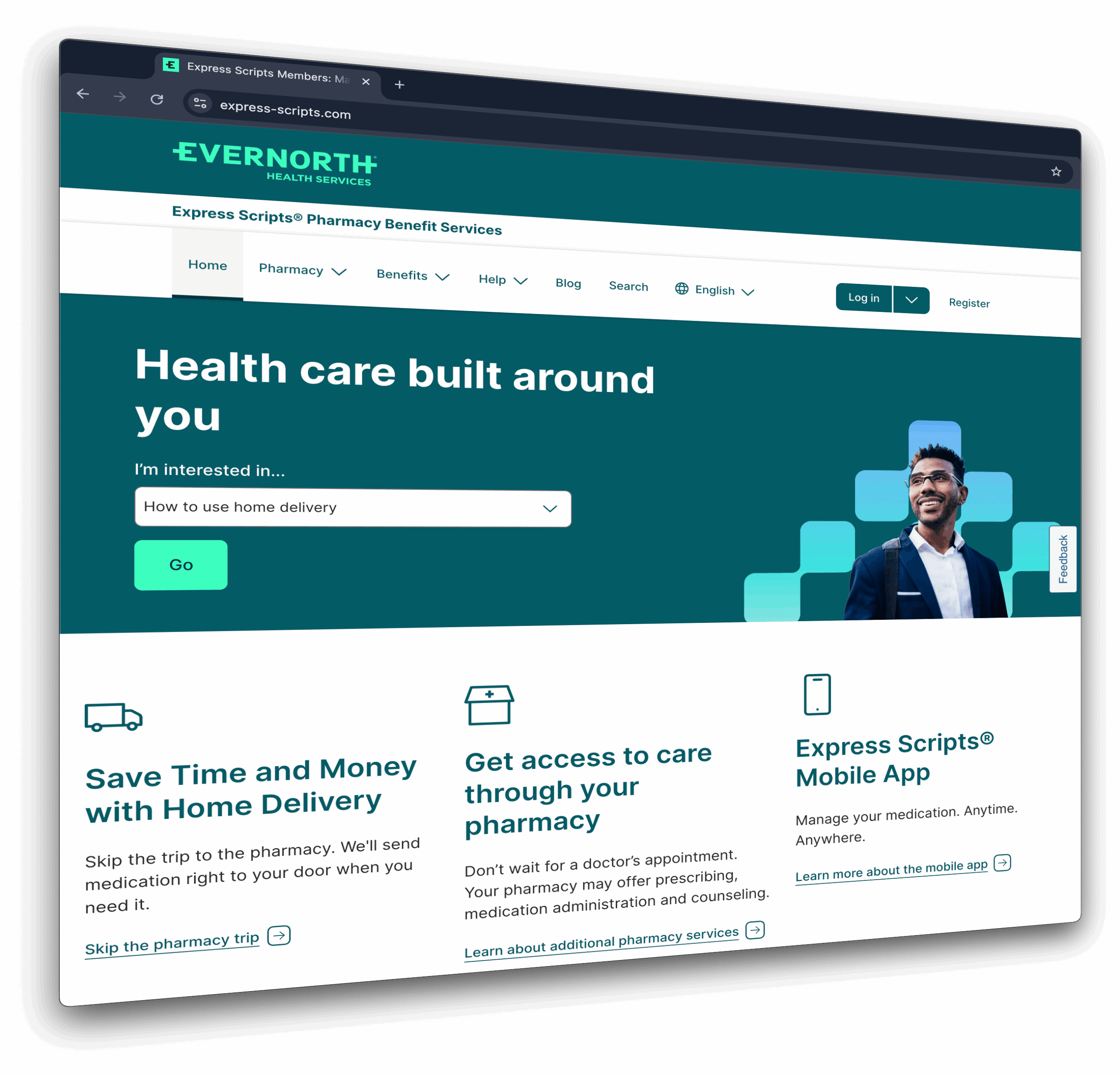 Express Scripts is the pharmacy benefit manager or administrator of our drug benefit program. Evernorth is the parent company of Express Scripts. You may start seeing the name Evernorth more often. Nothing is going to change as far as the way you access your pharmacy benefit. We simply want to make you aware so when you start seeing the name Evernorth you won't be confused.
Express Scripts is the pharmacy benefit manager or administrator of our drug benefit program. Evernorth is the parent company of Express Scripts. You may start seeing the name Evernorth more often. Nothing is going to change as far as the way you access your pharmacy benefit. We simply want to make you aware so when you start seeing the name Evernorth you won't be confused.
If you have any questions, please contact Insurance Services at insurance@jordandistrict.org or 801-567-8146 and we will be happy to assist you.
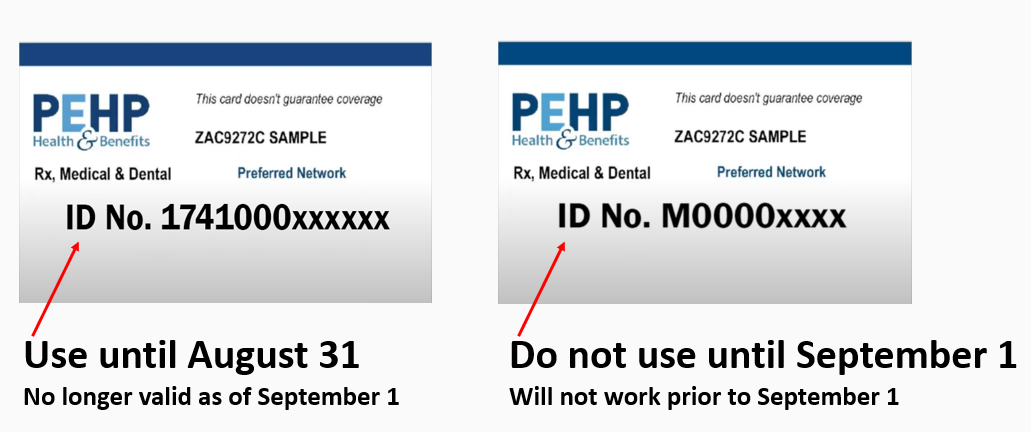
PEHP Letter & ID Cards
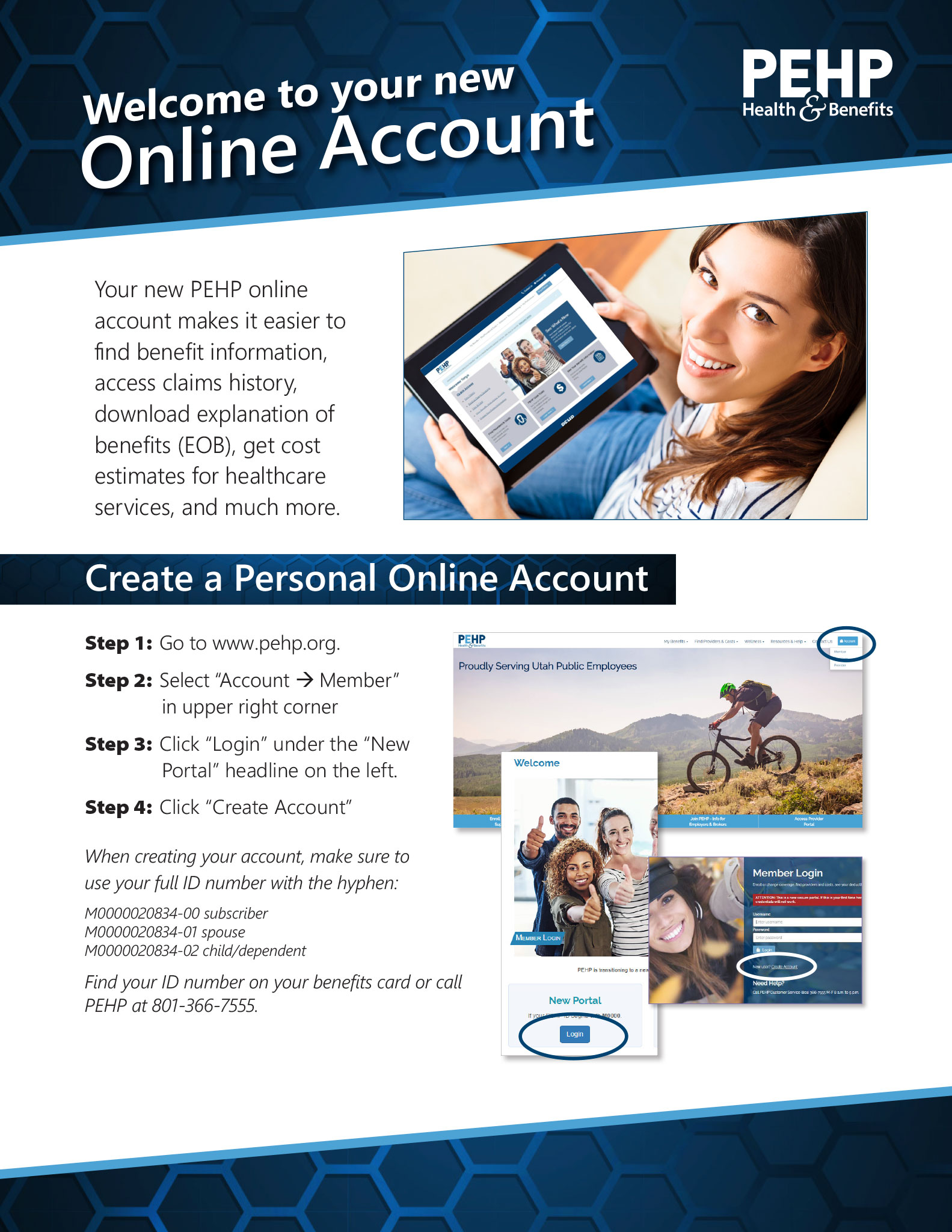 If you are enrolled in Jordan School District's medical plan, please check your mail for a letter from PEHP. They will start to mail these out today, Thursday, Aug. 21. This letter will include your new ID number which will start with the letter "M". This is not your card, just the letter that provides your new member ID number. Our members should start receiving their cards late next week.
If you are enrolled in Jordan School District's medical plan, please check your mail for a letter from PEHP. They will start to mail these out today, Thursday, Aug. 21. This letter will include your new ID number which will start with the letter "M". This is not your card, just the letter that provides your new member ID number. Our members should start receiving their cards late next week.
Attached are the instructions that will walk you through how to create your new online account with PEHP. Starting September 1st, you can use your new member ID number to create an account in the new PEHP portal. Once you have your account set up, you will have the ability to print your ID card should you not receive it prior to September 1, 2025. Due to PEHP transitioning all members to their new system, there may be challenges.
We have had several members contact us because their providers office is adamant that they need to provide them with a new ID number. If this happens to you, please make them aware that you will be moving to the new system effective September 1, 2025 and will provide them with your new card once you receive it. They can also contact PEHP directly to confirm this information. It is very important that once September 1st is here that you are presenting the new card whenever you receive services. If you don't, it is going to create billing issues and the payment of your claim will be delayed. This needs to occur at the pharmacy as well. If you use your old card after August 31 it will show that you no longer have coverage.
Here is a picture of each of the cards so you know what to look for.
If you need assistance or have questions, please contact Insurance Services at insurance@jordandistrict.org or 801-567-8146.
Update: Express Scripts & Kroger/Smith’s Pharmacies
 Good news! Smith's pharmacy has once again contracted with Express Scripts (ESI) for our prescription drug plan. Please remember you can visit ESI's website or GoodRx and compare costs at a variety of local pharmacies.
Good news! Smith's pharmacy has once again contracted with Express Scripts (ESI) for our prescription drug plan. Please remember you can visit ESI's website or GoodRx and compare costs at a variety of local pharmacies.
If you have any questions, please visit Insurance Services website or contact them directly insurance@jordandistrict.org / 801- 567-8146.
Having a Baby? Or Any Other Qualifying Event?
You have 30 days to make those changes to your plan. IRS regulations govern how and when an employee may make cafeteria plan elections and changes to those elections.
If you have questions about what a qualifying event is, please click here.

